Coronavirus analysis
Expert view: Dr. David Heymann on the coronavirus outbreak
Medical experts around the world are scrambling to both contain and combat the new coronavirus from China. While the World Health Organization says that the new virus is not yet a pandemic, defined as ‘the worldwide spread of the new disease’, its high transmissibility has now resulted in 31,515 confirmed cases in 26 countries.
In a bid to learn more about the coronavirus outbreak, its possible impact, and the response required by the wider travel retail industry, The Moodie Davitt Report this week hosted a phone-in audience with public health expert Dr. David Heymann, who headed the global response to SARS in 2003. We present the key takeaways as well as highlights of an insightful question and answer session.

Dr. David Heymann is Professor of Infectious Disease Epidemiology at the London School of Hygiene & Tropical Medicine and Head of the Centre on Global Health Security at Chatham House, London.
From 2012 to March 2017, Dr Heymann was chairman of Public Health England. Earlier in his distinguished career, he was Executive Director of the Communicable Diseases Cluster, and crucially, he headed the global response to SARS in 2003.
The key to understanding the 2019-nCoV virus
Medical experts now have more information on the transmissibility of the new virus but still need to determine the severity of the infection compared to viruses of the past. Data from China, the country of origin and location by far of the greatest number of cases confirmed, has not been made available in sufficient volume yet, with Chinese medical experts and authorities busy containing the virus and tending to those infected. According to Dr. Heymann, much more will be known about severity and containment as data is acquired from the countries outside China that the virus has so far reached.
Comparison with SARS and other past outbreaks
The new virus has shown more similarities with the MERS coronavirus that surfaced in the Middle East in 2012 than with SARS. The fatality rate is also more like MERS than SARS. Based on reported cases from China, the fatality rate of hospitalised patients for the new outbreak is around 2%; lower than the 9.6% recorded for SARS.
A key difference between the current outbreak and the SARS outbreak is the number of individual chains of transmission that are being recorded. SARS had very few patients setting off a chain of infection, but the latest information from China suggests that the reverse is true of the new coronavirus.
Past experience shows that the development of new drugs to combat ongoing outbreaks has been ineffective, according to Dr. Heymann. The SARS outbreak was contained well before such a drug was developed. While vaccines are being developed, they won’t be available to use in the next few months when they are most needed.
Peak of the crisis and the possibility of a short-term easing
There is no evidence to suggest that the virus’s peak may come soon, as has been declared in some quarters. With infections still on the rise and considering the evidence to hand, it is not possible to accurately predict either when the crisis will peak or how long it will last.
Question & Answer with Dr David Heymann
The Chinese Center for Disease Control and Prevention confirms 31,203 cases in Mainland China and a total of 636 deaths as of 7 February. The number of new confirmed cases continues to increase and shows little sign of easing. The number of new medical observations has stabilised however, instead of increasing on a day-by-day basis.
Here are the highlights from this week’s briefing.
Martin Moodie: The World Health Organization said yesterday that there is a “window of opportunity” to stop the novel coronavirus becoming a broader global crisis. You said this week that it was too early to estimate when the outbreak would peak as it appears to still be on the increase. Could you expand on that?
Dr. David Heymann: There are several factors required to understand this outbreak. That includes the transmissibility – the ability of the virus to spread from person to person; it includes the way the virus is transmitted from person to person; and the third factor that is not understood is the severity of the infection.
That data has not come out of China because there is quite a bit of work going on trying to take care of the number of patients they have.
That information will come out in the next few weeks and at the sites where the virus has been exported. As of today, there are 23 countries that have received this virus from patients in China. Nine of those countries have had human to human transmissions so we are beginning to understand better how this virus acts in the population.
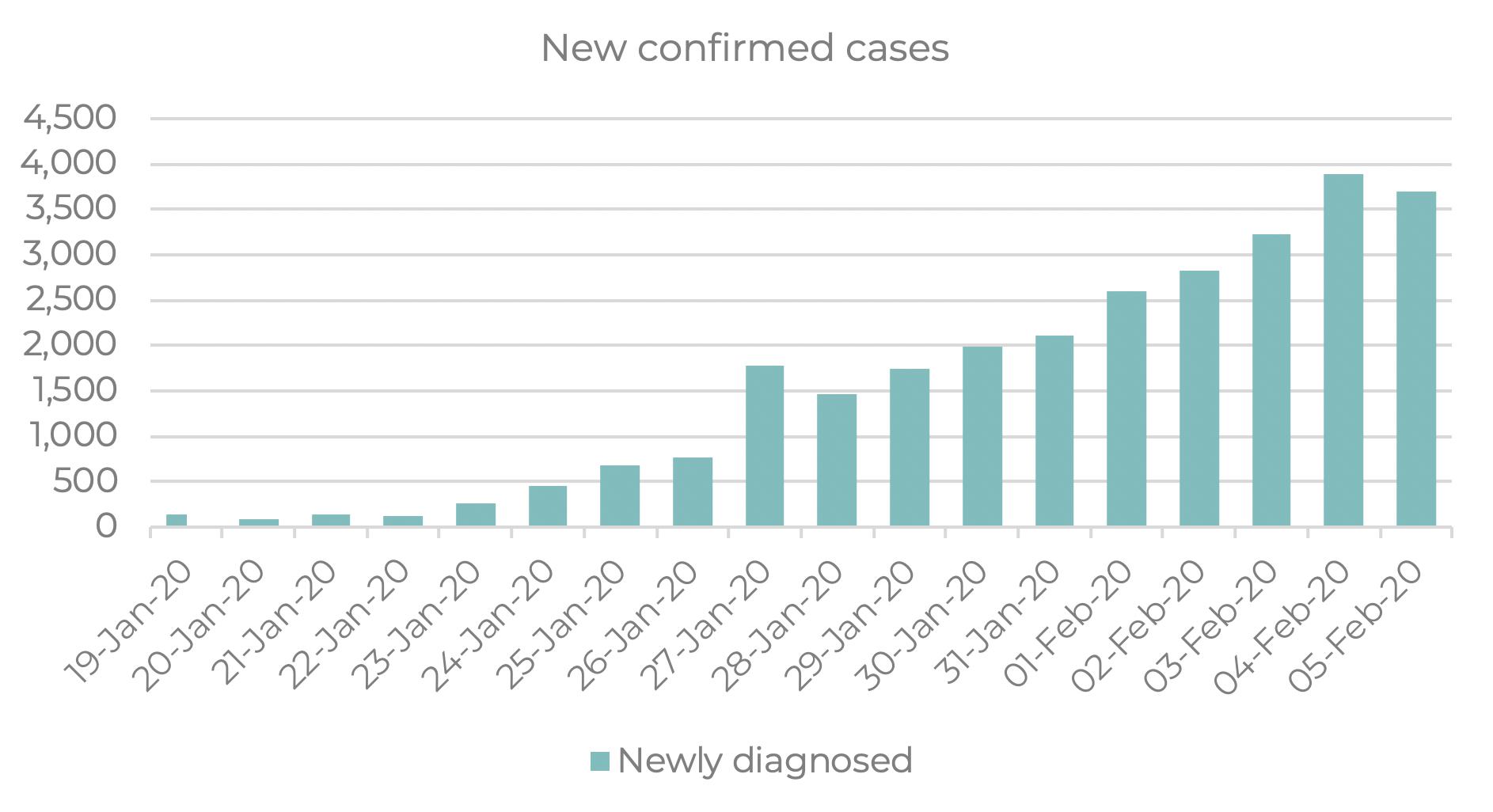
(Source: Chinese Center for Disease Control and Prevention, Moodie Davitt Business Intelligence Unit)

(Source: Chinese Center for Disease Control and Prevention, Moodie Davitt Business Intelligence Unit)
Martin Moodie: How important is it to compare the two outbreaks? And knowing what we know about SARS in 2002 and 2003, how important are the lessons of SARS in understanding the new coronavirus?
Dr. David Heymann: Initially the data that came out of China suggested they might be similar types of outbreak but that it might be less lethal and more related to the MERS coronavirus which came out of the Middle East. That hasn’t changed since then. It’s understood that this can be transmitted face to face and it can also be transmitted by close body contact or body fluids. It looks more like the MERS coronavirus than the SARS virus at this point in time in regards to mortality.
Those projections vary depending on what figures are used in the modelling. So it is really not possible at present to predict when this will be. What’s important though is to understand that this is different to the SARS outbreak. That began in 2002 with very few patients or even just one patient who began a chain of transmission which continued until it amplified under a hospital setting where workers were infected and spread it to hospital patients, families and communities.
The current outbreak started with an explosive beginning, from what we understand, with many people infected, each one of them setting off an individual chain of transmission. So that is what we are seeing now: family members in close contact developing the illness.
Martin Moodie: How important is it to compare the two outbreaks? And knowing what we know about SARS in 2002 and 2003, how important are the lessons of SARS in understanding the new coronavirus?
Dr. David Heymann: Initially the data that came out of China suggested they might be similar types of outbreak but that it might be less lethal and more related to the MERS coronavirus which came out of the Middle East. That hasn’t changed since then. It’s understood that this can be transmitted face to face and it can also be transmitted by close body contact or body fluids. It looks more like the MERS coronavirus than the SARS virus at this point in time in regards to mortality.
China is reporting fatal cases from among all the people who are infected and the spectrum of disease appears to be from very mild infection which causes symptoms of common cold, all the way through to pneumonia. If we put this in perspective, now they are reporting around 400 deaths and 20,000 confirmed cases.
In a country the size of China, that’s a small number of cases and deaths compared to the entire population of over a billion people. But it is very important because it’s a new virus among humans and its potential is not yet understood. So the fatalities are occurring but what’s not known is the denominator under those fatalities.
We know that in hospitalised patients, around 2% have mortality. But there is a whole spectrum of patients that never get into hospitals and aren’t reported as part of that denominator, which is the part necessary to understand the complete spectrum of disease and its mortality rate.
Martin Moodie: What do you feel about the chances of a vaccination and/or suitable treatment being developed in a timely manner to use against this coronavirus?
Dr. David Heymann: Currently there are some vaccines being developed but they won’t be in time to use in the next few months or so when there might be need of a vaccine. Antivirals are being tested in China, but there’s very little understood about what type of ethical clearance has been done and what the protocol is. I know the WHO is working with them to try to understand what they are doing and they are doing some clinical trials with drugs coming from major pharmaceutical companies.
Martin Moodie: Does that mean therefore that this effectively will run its course, whatever that course may be?
Dr. David Heymann: There is a basic approach in containing an outbreak and that’s what’s being done in countries where the virus has landed outside of China. Those countries are tracing all contacts and making sure that those contacts are either remaining at home or in a quarantined facility.
Temperatures are being checked daily and should patients develop a temperature they are diagnosed. If they are found to be positive for infection they are placed under isolation in hospital.
They are also identifying other patients who might be infected in their countries and they are isolating them as well. So isolation of patients, tracing of contacts and making sure patients are treated properly is a way an outbreak can be stopped. We’ll see whether that’s successful in countries where the virus has landed from China, but it is difficult to understand what’s going on in China because of all the cases and the widespread outbreak.
Martin Moodie: You were in the front line during the SARS outbreak. How does the handling of the new outbreak compare with the past?
Dr. David Heymann: I have privileged access because I chair an advisory group for the World Health Organization that advises the emergencies programme. From that point of view, we see documents that are coming regularly to the World Health Organization, providing updates. Sometimes they don’t provide all the information necessary to do a proper risk assessment because they are doing many things at one time. But the 23 countries outside of China where the outbreaks are occurring will be very important to understand the outbreak and the virus spread.
Martin Moodie: China has been the source of a lot of major outbreaks, such as Avian Flu, SARS and now the Coronavirus. Given the importance of the Chinese to the global travel market, do you think China will continue to be the country of origin for repeated outbreaks in the future?
Dr. David Heymann: That depends on what happens after this outbreak. These outbreaks are associated with the sale of live animals used for food. There are some ways that this can be dealt with. Certainly China will now attempt to regulate the sale of these animals, but without proper enforcement that could even be worse because it could drive the trade underground. There are other methods, such as domesticating wild animals and making sure they are raised under sanitary conditions so they won’t cause a problem. In Hong Kong, when there was an outbreak of avian influenza in 1997, they stopped live animal sales of chicken. So there are ways of dealing with this and I think China will be considering that as they go forward. For the industries in China it will be important to consider what the opportunities are as time goes on.
Martin Moodie: The audiencelistening to this call is linked inextricably to the travel and tourism sector. In your view, is there a strong argument for curbing travel or even cross border travel by land? Is that an effective measure?
Dr. David Heymann: The WHO has made some recommendations and those recommendations were that travel and trade does not need to be affected at this point in time. That’s a recommendation to countries, but countries will make their own decision as does the private sector.
Countries use information from WHO with their own risk assessment and make their own decisions based on that assessment and their needs. The private sector not only includes WHO’s recommendations but also other factors such as insurance and worker safety. These decisions are made by the private sector and there are other influences on them other than just the risk assessment.
We know that temperature screening does not pick up all cases and all infections because people cross the border in their incubation period and develop the disease after they are in the country. We have seen that in many different countries. So although temperature screening might identify a few patients and provide for them an earlier diagnosis and possibly better management of their infection, it’s not a way of stopping the disease from entering your country.
In a country, there must be good disease detection systems which will identify this infection early and diagnose it and take proper precautions. There are other advantages to screening at airports and providing that to all people coming from where the outbreak is occurrin. Those advantages include the information they need to know if they might have developed the disease and where to report if the disease has occurred. So there are many different approaches that various countries use and this is a national decision.
It’s important for the tourism and retail industry to understand what happens when there are cases that occur, such as has happened on a couple of cruise ships where there has been a quarantine of those ships. It’s important to take that into the risk assessment. I can’t give a formula but every company in the industry must take into account the risk assessment done by the WHO, the understanding of the virus and where it’s coming from and make decisions based on insurance and other safety precautions required.
Dermot Davitt (leading audience Q&A): According to the Center for Disease Control, in the 2017-18 flu season in the USA more than 900,000 people were hospitalised and there were over 80,000 deaths. Please put the coronavirus in context of this.
Dr. David Heymann: Influenza is transmitted in a different way to how we believe this coronavirus is transmitted. Influenza is transmitted through coughs or sneezes; it puts out an aerosol that can travel within a closed area or across a table and infect others. It’s much more infectious, at least from what we understand of the current virus. It’s important to note that influenza is a very serious illness for the elderly and those with co-morbidity such as diabetes or lung disease. The same appears to be true for this coronavirus where the elderly with co-morbidity have an increase in mortality.
So putting this in perspective, with 20,000 confirmed cases in China of a population of over a billion; that pales in light of when influenza occurs and spreads very easily from person to person. The new coronavirus, as we understand it now, can only be transmitted by very close face to face contact and heavier water particles – droplets rather than aerosol.
Dermot Davitt: There have been reports that the virus can remain active on surfaces for long periods suggesting that there is a high risk of contagion. Does this mean that contagion is likely to be much greater than SARS, even if the mortality rate is lower?
Dr. David Heymann: Theoretically if someone coughs or sneezes on a door knob or somewhere else, the virus can remain active as long as the virus is surrounded by water; by the secretion. When that dries the virus can no longer survive and it is no longer infectious. It’s always a wise policy to make sure hands are washed whenever you deal with other people – including shaking hands – when there is an outbreak such as this.
Dermot Davitt: What measures can the tourism and retail industry adopt in practical terms to help stem the outbreak?
Dr. David Heymann: It’s important for the tourism and retail industry to understand what happens when there are cases that occur, and it’s important to take that into account in the risk assessment. I can’t give a formula for that, but every company must take into account the risk assessment done by the World Health Organization, have an understanding of the virus and where it is coming from, and make decisions based on insurance and other required safety precautions.
Dermot Davitt : What will be the signs that the virus is slowing down its spread? What numbers should we be watching?
Dr. David Heymann: What we are seeing is that it continues to increase, or at least the reports are increasing. That means the Chinese are looking for cases, finding those cases and reporting those cases. It’s very difficult to say when the epidemic will peak in China.
What we need to watch also is what’s happening in the 23 states outside of China where the virus is known to be present. If they are successful in containing the virus and not seeing it spread out of the immediate area where the cases have been imported, that will be a sign that the outbreak can be contained and possibly a pandemic will not occur.
When a new organism emerges from an animal to a human, there are three possible ways it can act. First is by causing disease and spreading further; a good example is rabies. The second is it spreads from person to person through body secretion or close contact and it disappears; this is true with Ebola and Avian Influenza. And then there are viruses that enter the human population and become endemic in those populations; a good example of that is HIV.
What’s important now is to understand the potential of the virus. It appears it may be like the Ebola virus, Avian Influenza virus, like SARS and something which will not become endemic. It’s not yet clear that that’s the case. We have to be watching those places where there is extreme control now because of the small number of cases.
Martin Moodie: Given the spread of infections over the recent weeks, there is a delay between infection and illness and, eventually death. As the virus spreads, are the mortality rates likely to ‘catch up’?
Dr. David Heymann: What is most likely is as the virus continues to spread is that there will be a broader spectrum of disease. Remember the majority of these infections are not lethal. What is not known is how many of these infections are asymptomatic or have very slight symptoms which are similar to a common cold.
It’s important to understand the case definition being used in China. The definition defines what a case is and permits you to identify cases. Cases that meet the definition or persons that fit the definition are called a case. In China, until recently and possibly still, they use pneumonia in their case definition. Pneumonia is a severe form of the disease and probably not occurring in the majority of the patients. But that’s a denominator they are using to calculate their mortality.
Dermot Davitt: When do you think any travel bans can and should be lifted?
Dr. David Heymann: That I can’t predict and I don’t think anybody can. Travel bans occur as a precautionary measure when the organism or disease is not completely understood. With the SARS outbreak, it was understood the transmission was face to face as it appears with this outbreak.
What happened in Hong Kong was that there was an apartment complex where over 200 cases were confirmed. It was not understood why they were occurring and traced back to another case. It was assumed there was another environmental factor in addition to the human to human.
So other countries that were not able to trace back their patients with other patients who had the infection were presumed to have environmental transmission and it was recommended to postpone travel there. As soon as it was understood how transmissions were occurring in Hong Kong, the travel restrictions were lifted. They were precautionary measures as a means to prevent anything that might be in the environment. So that is why travel bans are set in place. As countries understand more about their virus they will reconsider what they are recommending, as will airlines and other companies.
*This feature contains edited highlights; a full transcript of the call with Dr. David Heymann is being provided to all those who dialled in on 5 February.

The Moodie Davitt eZine
Issue 276 | 7 February 2020
The Moodie Davitt eZine is published 20 times per year by The Moodie Davitt Report (Moodie International Ltd).
© All material is copyright and cannot be reproduced without the permission of the Publisher.
To find out more visit www.moodiedavittreport.com and to subscribe, please e-mail sinead@moodiedavittreport.com

